
Living with chronic pain can be debilitating and impact one’s quality of life. Fortunately, advancements in pain management have led to innovative treatments, one of which is pulsed radiofrequency (PRF) therapy. In this blog, we will explore the latest research surrounding the use of PRF for the treatment of lateral cutaneous nerve of the thigh (LCN) pain. Let’s delve into the world of PRF and its potential benefits for those suffering from LCN-related discomfort.
Understanding Pulsed Radiofrequency Therapy
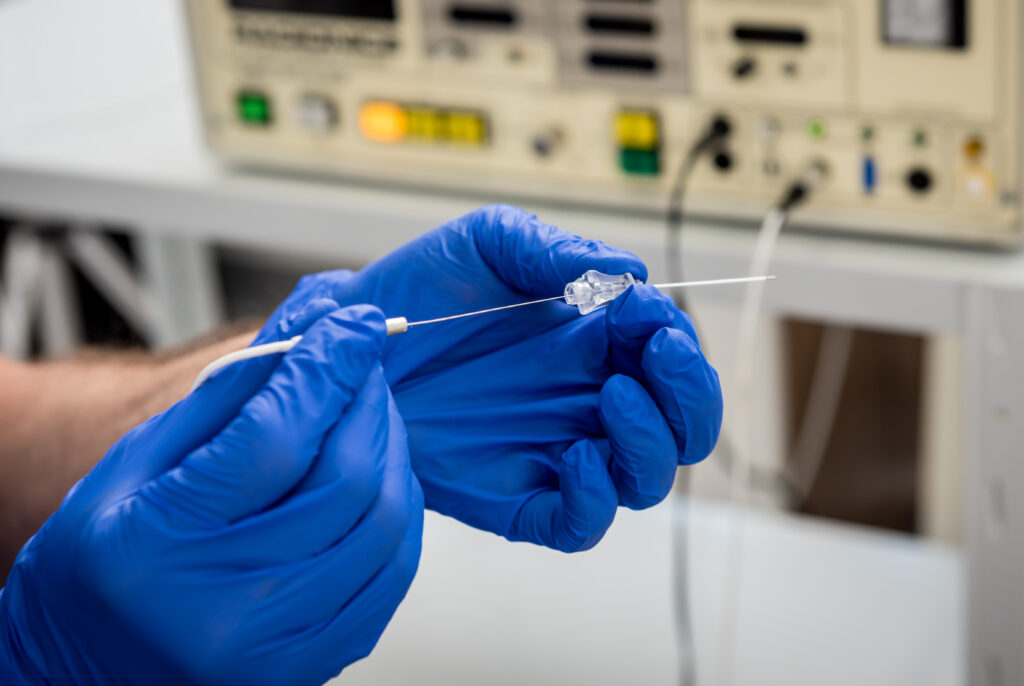
Pulsed radiofrequency therapy is a non-invasive treatment approach that specifically targets and modulates the activity of nerves to relieve pain. It involves the application of low-intensity electrical pulses directly to the affected nerves. By delivering these pulses in a pulsatile manner, PRF aims to disrupt the transmission of pain signals, offering a potential method for pain management.
Unlike continuous radiofrequency therapy, which generates heat to create a thermal lesion on the nerves, PRF utilizes brief bursts of energy. This unique characteristic of PRF minimizes the risk of tissue damage and allows for a more controlled and precise treatment. The pulsatile nature of PRF enables the modulation of nerve activity without causing thermal injury, making it a safer option for patients.
The therapeutic effects of PRF are thought to be multifactorial. By modulating the activity of nerves, PRF can potentially interrupt or modify the transmission of pain signals to the brain, resulting in pain relief. Additionally, PRF may also have anti-inflammatory effects, helping to reduce pain and inflammation in the targeted area. The exact mechanisms of action of PRF are still being studied and understood, but its potential to offer pain relief with minimal risk of tissue damage makes it an intriguing option for patients seeking alternative pain management approaches.
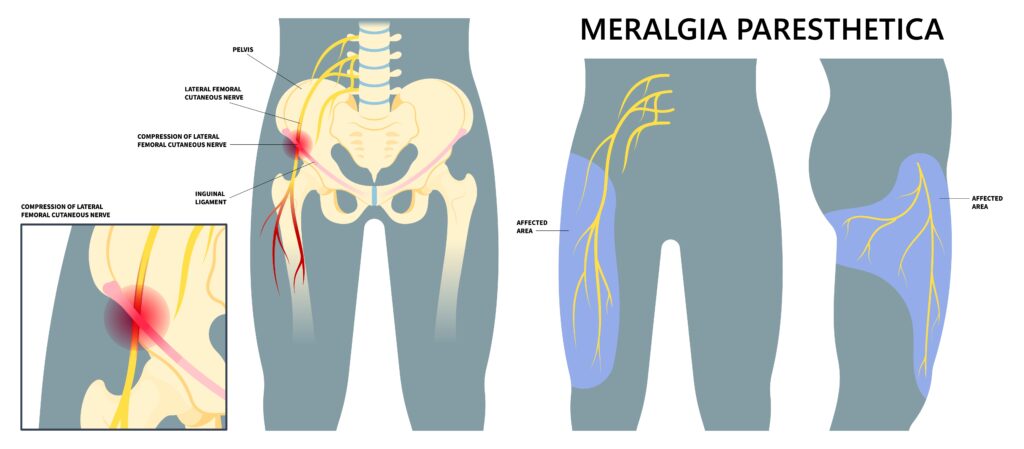
Lateral Cutaneous Nerve of the Thigh Pain
LCN pain, also known as meralgia paresthetica, is a condition that manifests as tingling, numbness, and burning sensations in the outer thigh. It occurs due to compression or irritation of the lateral cutaneous nerve of the thigh (LCN), which is responsible for supplying sensory fibers to the skin of the lateral thigh.
There are several factors that can contribute to the development of LCN pain. One common cause is obesity, as excess weight can put pressure on the LCN, leading to symptoms. Additionally, wearing tight clothing, such as belts or pants, can also compress the nerve and result in discomfort. Trauma, such as injury or surgery, can damage the LCN and cause pain as well. Finally, individuals with diabetes may be at a higher risk for LCN pain, as the condition can affect nerve function.
Treatment options may include conservative measures such as wearing looser clothing, weight management, and physical therapy exercises to alleviate pressure on the nerve. In some cases, medications or injections, such a local anaesthetic injections or pulsed radiofrequency treatment may be recommended to manage pain.
Efficacy of PRF for LCN Pain
Recent studies have highlighted the efficacy of PRF in managing LCN pain. Research published in PAIN MEDICINE has reported successful treatment outcomes, including complete and sustained relief of thigh pain following PRF therapy. Another study from Regional Anaesthesia and Pain Medicine demonstrated the benefits of ultrasound-guided PRF ablation of the LCN for treating meralgia paresthetica.
Mechanisms of PRF and Pain Relief
The exact mechanisms by which PRF alleviates pain are still being elucidated. However, it is believed that the electrical pulses disrupt the abnormal transmission of pain signals, modulating the activity of pain-sensitive nerve fibers. This modulation can lead to reduced pain perception and improved function.
Considerations and Side Effects
PRF therapy is generally considered safe and well-tolerated. However, like any medical procedure, there are potential side effects and contraindications. Common side effects include temporary skin numbness, mild discomfort at the treatment site, and mild bruising. It is crucial to consult with a qualified pain specialist to assess the appropriateness of PRF therapy based on individual circumstances.
Summary and Recommendations
Pulsed radiofrequency therapy holds promise as a non-invasive and effective approach for managing LCN pain. Research published in reputable journals such as PAIN, PAIN MEDICINE, and Regional Anaesthesia and Pain Medicine supports the use of PRF for treating LCN-related discomfort. However, it is essential to consult with a pain specialist to evaluate suitability for treatment and discuss potential risks and benefits.
In conclusion, pulsed radiofrequency therapy offers hope to individuals suffering from lateral cutaneous nerve of the thigh pain. By utilizing this advanced technique, we can potentially alleviate their symptoms and enhance their overall well-being.
Remember, seeking personalized medical advice from a qualified professional is crucial before considering any treatment option.
References
- Park D, Chang MC. The mechanism of action of pulsed radiofrequency in reducing pain: a narrative review. J Yeungnam Med Sci. 2022 Jul;39(3):200-205. doi: 10.12701/jyms.2022.00101. Epub 2022 Apr 7. PMID: 35385898; PMCID: PMC9273139.
- Rollin M. Gallagher, MD, MPH, Pulsed Radiofrequency Treatment: Biological Mechanisms and Clinical Evidence, Pain Medicine, Volume 6, Issue 6, November 2005, Pages 401–402, https://doi.org/10.1111/j.1526-4637.2005.00077.x
- Alaa Abd-Elsayed, MD, MPH and others, Lateral Femoral Cutaneous Nerve Radiofrequency Ablation for Long-term Control of Refractory Meralgia Paresthetica, Pain Medicine, Volume 21, Issue 7, July 2020, Pages 1433–1436, https://doi.org/10.1093/pm/pnz372
- Fowler IM, Tucker AA, Mendez RJ. Treatment of meralgia paresthetica with ultrasound-guided pulsed radiofrequency ablation of the lateral femoral cutaneous nerve. Pain Pract. 2012 Jun;12(5):394-8. doi: 10.1111/j.1533-2500.2011.00522.x. Epub 2011 Dec 7. PMID: 22151457.
- Van Zundert, Jana,d,*; Patijn, Jacoba; Kessels, Alfonsb; Lamé, Ingea; van Suijlekom, Hansc; van Kleef, Maartena. Pulsed radiofrequency adjacent to the cervical dorsal root ganglion in chronic cervical radicular pain: A double blind sham controlled randomized clinical trial. Pain 127(1):p 173-182, January 2007. | DOI: 10.1016/j.pain.2006.09.002

Dr. Ilonka Meyer is the Clinical Director and Founder of MindBodyPainSpecialists. She also holds an appointment as Acting Director of the Pain Service and Pain Specialist at the Austin Hospital in Heidelberg, Melbourne. Ilonka has a strong interest in interventional pain treatments, peri-operative pain and medication optimisation and cancer pain.
Ilonka is skilled in Clinical Research, Medical Education, Coaching, and Healthcare Management. Her main research focus lies in interventional pain medicine in the peri-operative population, cancer pain and the health economic benefits of pain and medication optimisation in patients both pre-and postoperatively.


