
Chronic pain is a persistent problem for many people. According to the Australian Institute of Health and Welfare, one in 5 Australians aged 45 and over are living with persistent, ongoing pain. Current treatments for chronic pain often come with unpleasant side effects or the risk of drug interactions, so there is a great need for new and effective therapies.
Palmitoylethanolamide (PEA) is a natural fatty acid that has analgesic, anti-inflammatory, and neuroprotective effects. In this blog post, we will discuss the current research on PEA and its potential as a treatment for chronic and neuropathic pain (nerve pain).
Palmitoylethanolamide (PEA) is present in all mammals, including humans. It is produced naturally in the body and is also found in some foods, such as chicken egg yolk and soybeans.
What is PEA?
Palmitoylethanolamide (PEA) is a fatty acid amide that is naturally produced in the body. PEA is found in high concentrations in the central nervous system. It is produced by neurons, glial cells, and immune cells. PEA belongs to a class of endocannabinoids known as N-acylethanolamines (NAEs).
How does Palmitoylethanolamide (PEA) work?
PEA binds to both CB1 and CB2 receptors, although its binding affinity is higher for CB2 than for CB1. The activation of CB2 receptors by PEA is thought to be responsible for the management of pain. Research suggests that PEA may be an effective treatment for neuropathic pain, inflammatory pain, and neuro-inflammatory conditions.
PEA functions as an agonist at both TRPV1 and TRPA1 ion channels.TRPV1 ion channels are located on nociceptive neurons and are activated by noxious stimuli such as heat, acidic pH, and capsaicin. Activation of TRPV1 ion channels results in an influx of calcium ions into the cell, which leads to the initiation of pain signals.
TRPA1 ion channels are also located on nociceptive neurons and are activated by noxious stimuli such as cold temperatures and mustard oil derivatives. Activation of TRPA1 ion channels also results in an influx of calcium ions into the cell, which leads to pain signals being transmitted from the periphery to the central nervous system.
You may have heard of the endocannabinoid system (ECS), but what exactly is it and how does it work?
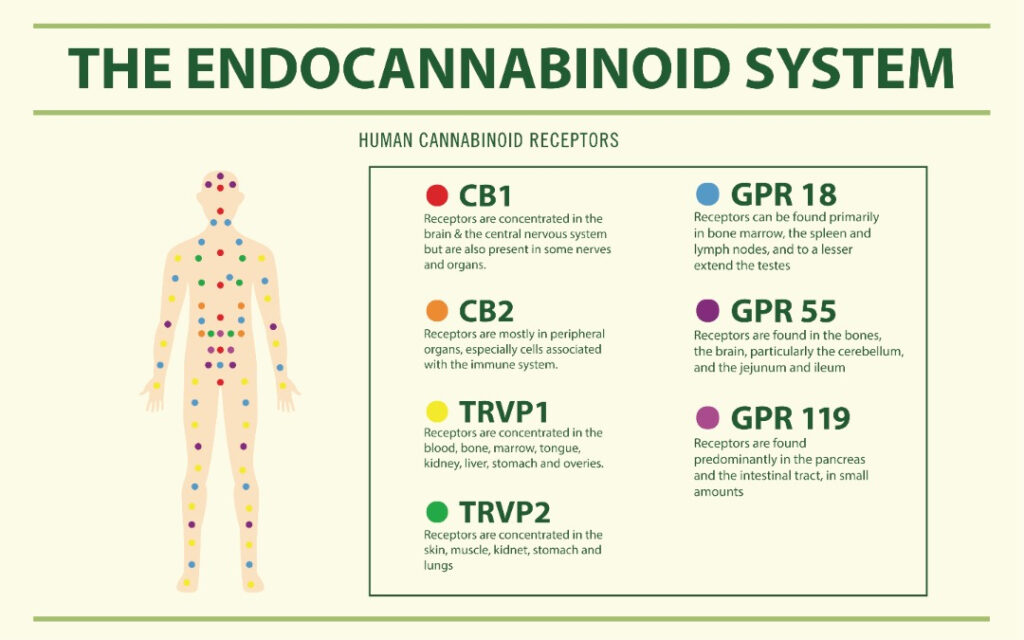
The ECS is a complex cell-signaling system that plays a role in maintaining homeostasis in the body. This system is involved in many physiological processes, including regulating many important functions in the body including pain, inflammation, mood, and sleep.
The ECS is made up of endocannabinoids, which are ligands that bind to cannabinoid receptors. There are two known cannabinoid receptors, CB1 and CB2. CB1 receptors are found primarily in the brain and central nervous system, while CB2 receptors are found mainly in the peripheral nervous system. Both CB1 and CB2 receptors are G protein-coupled receptors (GPCRs).
The CB1 and CB2 receptors are activated by endogenous ( produced naturally by the body) and exogenous (plant-derived) cannabinoids. The activation of CB1 receptors is primarily responsible for the psychoactive effects of cannabinoids, while CB2 activation is thought to be responsible for the immunomodulatory and anti-inflammatory effects.
What Does the Research Say?
There is a growing body of evidence from clinical trials supporting the use of PEA as a treatment for chronic and neuropathic pain. A number of studies have shown that PEA supplements can help to reduce pain and improve the quality of life in people with chronic pain.
One study in cancer patients found that PEA was effective at reducing neuropathic pain when used alongside standard pain medication. Another study found that PEA was effective at reducing inflammatory joint pain in patients with rheumatoid arthritis.
A 2017 systematic review looked at 28 clinical trials on the efficacy of PEA for treating various types of chronic and neuropathic pain. The authors concluded that “PEA is an effective adjuvant therapy for chronic non-cancer related pains.”
Another study published in 2018 found that PEA was an effective treatment for nerve damage-related pain reduction. The authors conclude that “PEA should be included in guideline-recommended pharmacological treatments for diabetic patients with painful diabetic neuropathy.”
A recent study by Austrian researchers, published in 2022, concluded PEA has clinically relevant analgesic properties, acting on both peripheral and central mechanisms (reducing wind-up) as well as in pain modulation, therefore increasing pain tolerance.

What conditions might be improved by taking PEA as a supplement?
Conditions where people might benefit from using PEA for their pain management include (but are not limited to):
- Neuropathic pain (nerve pain)
- Inflammatory pain
- Fibromyalgia
- Radiculopathic pain
- Peripheral neuropathy
- Persistent post-surgical pain
- Chronic pelvic pain
- Visceral pain
- Diabetic neuropathy
How long does it take to see an effect after starting PEA?
Individual patients can take up to 4 – 6 weeks to experience benefits from PEA supplementation. It is well tolerated and has no known side effects which makes PEA an option for patients who have multiple medication sensitivities or allergies.
Conclusion:
Although more research needs to be done on PEA and its potential therapeutic applications, current evidence suggests that PEA holds promise as a treatment for chronic pain conditions due to its ability to modulate both TRPV1 and TRPA1 ion channels.
The current emerging evidence and clinical data suggest that PEA may be an effective treatment for treating chronic pain with few side effects. If you are interested in trying PEA, speak to your healthcare provider about whether it is right for you.
Disclosure: The information in this article is not intended to replace your doctor’s medical advice, diagnosis or treatment. If you require more information, or have any questions, please speak to your doctor/ specialist.
References:
- Artukoglu BB, Beyer C, Zuloff-Shani A, Brener E, Bloch MH. Efficacy of Palmitoylethanolamide for Pain: A Meta-Analysis. Pain Physician. 2017 Jul;20(5):353-362. PMID: 28727699.
- Guida, F., Luongo, L., Boccella, S. et al. Palmitoylethanolamide induces microglia changes associated with increased migration and phagocytic activity: involvement of the CB2 receptor. Sci Rep 7, 375 (2017). https://doi.org/10.1038/s41598-017-00342-1. https://rdcu.be/cZxUt
- Petrosino S, Di Marzo V. The pharmacology of palmitoylethanolamide and first data on the therapeutic efficacy of some of its new formulations. Br J Pharmacol. 2017 Jun;174(11):1349-1365. doi: 10.1111/bph.13580. Epub 2016 Sep 29. PMID: 27539936; PMCID: PMC5429331.
- The Effect of Palmitoylethanolamide on Pain Intensity, Central and Peripheral Sensitization, and Pain Modulation in Healthy Volunteers—A Randomized, Double-Blinded, Placebo-Controlled Crossover Trial Kordula Lang-Illievich, Christoph Klivinyi, Gudrun Rumpold-Seitlinger, Christian Dorn and Helmar Bornemann-Cimenti. Nutrients 2022, 14, 4084. https://doi.org/10.3390/ nu14194084.
- https://www.metagenicsinstitute.com/ce-education/science-sheets/ecs-and-pea/#:~:text=%E2%9C%93%20PEA%20supports%20the%20ECS,and%20indirectly%20activating%20cannabinoid%20receptors.

Dr. Ilonka Meyer is the Clinical Director and Founder of MindBodyPainSpecialists. She also holds an appointment as Acting Director of the Pain Service and Pain Specialist at the Austin Hospital in Heidelberg, Melbourne. Ilonka has a strong interest in interventional pain treatments, peri-operative pain and medication optimisation and cancer pain.
Ilonka is skilled in Clinical Research, Medical Education, Coaching, and Healthcare Management. Her main research focus lies in interventional pain medicine in the peri-operative population, cancer pain and the health economic benefits of pain and medication optimisation in patients both pre-and postoperatively.
